supraventricular tachycardia
First Glance:
From across the room it looks like a fast and irregular narrow complex tachycardia.
Discussion:
This one isn’t easy to differentiate. Of the myriad flavors of SVT, I have no confidence that I could tell what it is from this strip. On the menu are a grab bag of afib, reentry and ectopic atrial tachycardias, atrial flutter and ‘fib-flutter’, sinus tachycardia with PACs, multifocal atrial tachycardia, junctional tachycardia, and tachy-brady syndrome.
Let’s look at the rates. Early in the strip it’s running around 140 bpm. Then it jumps midways to around 165, then to 215 for the last 11 beats before it converts suddenly to (presumably) sinus rhythm near the end of the strip. Remember that for this kind of rate calculation the instantaneous rate is 1500/# small boxes between QRS’s).
That bit of sinus is very helpful, as it gives us a clue as to what the native P wave looks like, so we might try to pick it out in the early rhythms to pick up on a sinus tachycardia. Unfortunately, it’s a soft P which is hard to differentiate from the T waves in SVT.
We can pick out some P waves in the early rhythms.
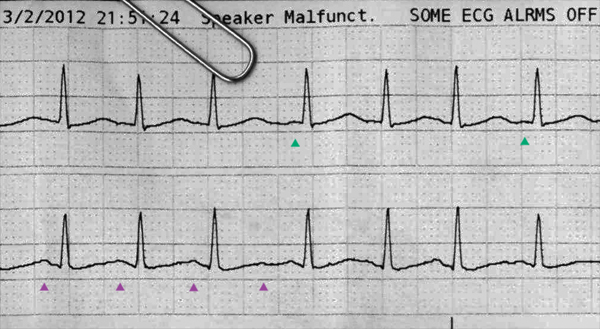
In teal we see a couple atrial waves. These are similar to the native P waves seen in the sinus rhythm, but the PR interval is too short. These are possibly ectopic atrial or- more likely- junctional beats. The QRS complex is identical to all other beats which proves they are all coming from above the split with the bundle branches. These could also be unusually organized atrial depolarizations in the setting of atrial fibrillation. The rhythm is quite irregular (which is harder to see as the rate increases) until the last run of 215 bpm beats (?re-entry cycle) before the final sinus rhythm.
In magenta we have some positive deflections after all beats. These are either T waves, or T waves with superimposed P waves as is common in fast sinus tachycardias. We just can’t know from this strip. You could look for other leads with more impressive P waves to try to elaborate this, and if it continued you could try getting a Lewis lead.
Final Impression?
Undifferentiated SVT to 215 bpm converting to sinus rhythm.
Management implications:
A tachycardia in the 200s is likely to have cardiac output ramifications for almost any patient, even those with healthy hearts, but this one is not sustained at that rate. If it gets up there and stays there, supportive treatment will be important, even if you have no firm diagnosis. Current ACLS guidelines support synced shocks for SVT with hemodynamic compromise (generally requires >150 bpm), with adenosine as an option while someone is looking for the pads. If nothing else, adenosine might depress the AV node enough for you to get a look at the atrial baseline and tell what is going on.
The Take-home Point:
There is a reason we call them ‘SVTs’. It’s a nice catch-all term for a difficult-to-differentiate group of rhythms. There are ways to tease them apart, either by adding more views (more leads, atrial-specific leads, even intra-cardiac leads using alligator clips and a central line) or by suppressing ventricular activity to see the baseline better. But don’t get caught up in diagnosis when you need to act now.
![]() Two star strip. The meat and potatoes.
Two star strip. The meat and potatoes.