irregular bradycardia
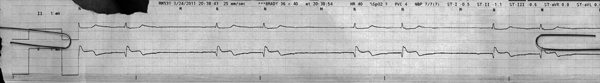
First Glance:
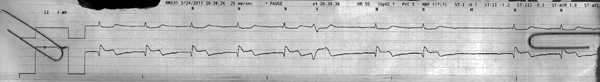
From across the room it looks like a wide-complex bradycardia with grouped beats.
Discussion:
Right off the beat, we can see this is probably a clinically significant rhythm. The complexes are wide and the rate is slow- about 40 bpm in this strip. All the complexes are identical, which makes me wonder if there is a blocked beat missing in the long pauses (2.2 seconds between beats).
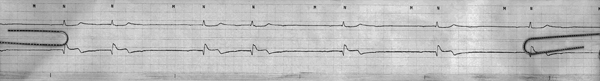
Look closely at the baseline:
Here we see regular bradycardic P waves with a long PR interval before every QRS, but one QRS is blocked creating each pause. This is a second-degree block.
If you look closely, and measure the PR interval, you see that the PR interval is longer in the second beat of every couplet, so this is a second degree type 1.
Here’s the rest of this same strip:
Here we see the 3:2 Wenkebach continuing until it switched to 2:1 halfway through. This is an even higher-grade block and is causing an even more severe bradycardia.
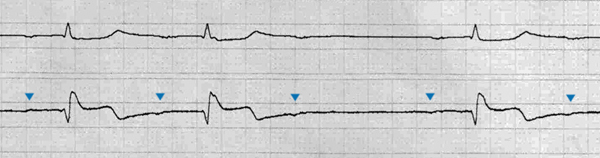
Here’s the strip from directly before the first strip I showed you:
Here we see 1:1 conduction for the first 5 beats, followed by a PVC with a compensatory pause (fancy way of saying it didn’t reset the sinus node), and then we see the previously discussed 2nd degree block come out.
All this is clearly grave electrical activity, with or without a pulse, and shows progressive dysfunction of the AV node.
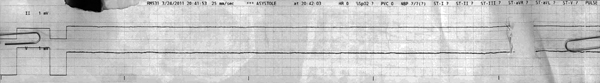
The next strip, from four minutes later:
Here we see the terminal rhythm: a baseline that still has the subtle regular P waves, but now nothing is conducting. This is complete heart block.
Anything we can say about the QRS complexes, at least when they were still around?
They are wide, with very subtle ST changes, with biphasic T waves in the chest lead that could be Wellen’s sign.
Final Impression?
AV node dysfunction progressing to complete heart block, and complex morphology consistent with possible coronary ischemia.
Management implications:
If your patient has a progressive block, don’t wait for them to have no AV conduction to look for the pacer pads. If this patient were not actively dying with a DNR, he would have required interventions (and possibly chest compressions) well before the organized rhythm disappeared from the monitor, and given that his AV node and ventricles seem completely uninterested in scraping together an escape rhythm it suggests that even anticholinergics and sympathomimetics might not have done much. I suspect pacing would have been his only hope to stabilize his bleak physiologic picture while theoretical providers tried to sort out the underlying etiology.
The Take-home Point:
Poor cardiac output causes coronary ischemia. Coronary ischemia can cause all kinds of conduction abnormalities. Bradycardia and 2nd degree type 1 block are associated with inferior infarction.
![]() Two star strip. The meat and potatoes.
Two star strip. The meat and potatoes.