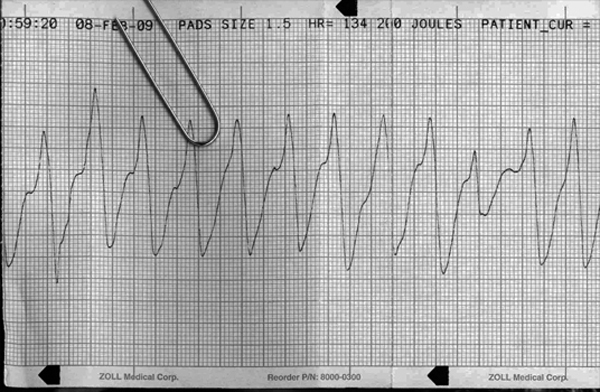
ventricular tachycardia
First Glance:
From across the room it looks like VT.
Discussion:
Finally, right? A straightforward ACLS strip. This is a wide complex tachycardia. We can’t see any obvious atrial dissociation (ie: regular P waves tracking through the strip) so I suppose this could also be a very aberrant supraventricular tachycardia, but its wild morphology and huge deflections have a very ventricular feel.
This is a strip from a Zoll brand monitor during a cardiac arrest. I believe the Zoll starts printing automatically when you start charging so we get these nice little code vignettes. We don’t have a calibration square, but we still know the voltage reference. The strip reads “PADS SIZE 1.5”. This means we are looking at the ‘pads’ lead at 1.5x standard calibration, which would mean 15 boxes per mV. The ‘pads’ lead is just using one pad (or paddle) as the negative electrode, and the other as the positive. If you put the pads on in the classic right upper chest/sternum to left lower axillary area you will get a lead that looks similar to lead II. Pads are far less likely to shake loose on your sweaty patient during CPR than some little EKG leads so is a great monitoring lead during resuscitations.
In this code situation if we have a pulseless patient showing this on the pads lead we don’t spend a lot of time thinking about the differential of wide complex tachycardias. However, in less urgent situations where management would change based on whether this was VT or SVT with aberrancy we could spend a lot of time sorting through complicated algorithms. One part of some of those algorithms is determining axis, which is always difficult for me with VT strips like this. You see a squiggly line. It is composed of two sets of spikes: one below the baseline, and one above the baseline. But where is the baseline? Which is which?
The way I think about it is as follows: The QRS is generally sharper. Here we see the upper row of spikes are sharper, so I am going to say that in this strip the QRS complexes are upright in the pads lead, and the negative spikes are the ST/T waves. Not useful here. Very useful when trying to calculate QRS axis for VT differentiation, however.
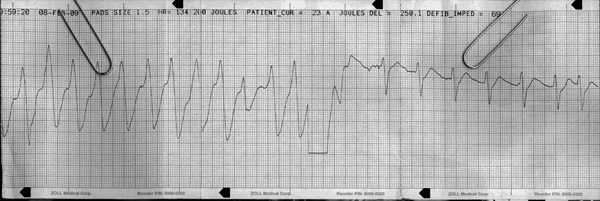
Halfway through the patient is defbrillated with return to a regular narrow complex rhythm. I don’t see P waves so it might not be sinus rhythm. We can pick out an unusually spiky T wave before the premature last beat of the strip, so this is a PAC. Given the P in that PAC is so well defined, and that this is probably lead II with 150% gain, it suggest there just aren’t P waves in the conversion rhythm so I would lean towards an accelerated junctional rhythm for this post-defibrillation strip.
Final Impression?
VT @ ~130 bpm (defibrillated with conversion to regular narrow complex rhythm with one PAC).
Management implications:
VT is a serious rhythm, and here we can see that it was serious enough in this patient that the providers deemed it worth shocking. What that means is that this was (hopefully) pulseless VT.
Your management of VT is not based only on the fact that it is VT. The first crucial step after identifying VT is seeing whether you have a perfusing rhythm or not. If there is a pulse- don’t shock them with 200J like this strip shows- they will either need synchronized shocks or something from the drug box, depending on the clinical setting.
The Take-home Point:
The first step is check pulse. Don’t see VT and shock reflexively.
ACLS guidelines clearly say you go right into CPR after administering the shock, but when you stop to check a rhythm and see those regular narrow complexes on the monitor, that doesn’t mean stop CPR. There may or may not be a pulse, even if the heart has converted to an organized rhythm. One guy on the carotid. One guy on the femoral.
My favorite way to check pulse during a pulseless code is to find the femoral pulse during compressions, then maintain my fingers just there when they hold compressions for pulse/rhythm check. That means less hunting around in folds of fat while they may or may not have a pulse.
Pop quiz: When you’re putting in the crash femoral line during CPR, do you aim for the pulse, medial to it, or lateral to it?
My (editorial) answer: You break out the ultrasound machine and do the job right. There are several documented reports of femoral pulsations during CPR originating in the vein. If no ultrasound, err medially per usual but understand that if you end up working your way back laterally to the pulsatile vessel it just might be the vein not the artery. Or: you might be about to put all the epi into their right leg.
Personally, the ridiculous advantage you get from using ultrasound could make the fem line a breezy 30-second cinch like it is supposed to be, instead of the protracted four minute septic stabfest that most code groin lines I see actually devolve into.
![]() One star strip. Students should identify the rhythm correctly.
One star strip. Students should identify the rhythm correctly.