SVT
First Glance:
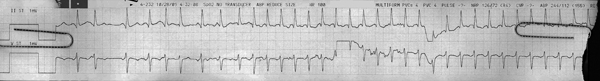
From across the room it looks like an irregular narrow complex rhythm that breaks into a regular SVT.
Discussion:
There are two chunks of strip that seem very different. The second chunk starts at beat 9 and is a regular supraventricular tachycardia @ 190 bpm. Like almost any SVT that fast it’s hard to decipher what’s going on. Let’s look at the first chunk and see if we can make some sense of this.
First, let’s see if we can pick out a native beat. Something that might be sinus. The best spot to look for something like that is after a stretch of flat baseline, where we are likely to see the native P wave. Beat 3 is this beat, and in lead II it has a positive P before it (normal), and a positive->negative (but predominantly negative) P in the chest lead (normal). The next QRS after beat 3 is far enough away that we also get a feel for what the native T wave looks like. It looks like this patient has T inversion in the chest lead, but this is normal in the septal leads, and I believe this is septal based on a few things:
1) The P wave in the chest lead looks septal (good evidence)
2) the axis looks normal in the septal leads, with a little R and a bigger S (weak circumstantial evidence)
3) nurses generally put the chest lead smack in the middle of the chest, which is septal (weak circumstantial evidence)
So what of the rest of the beats? Beat 1 looks like sinus, 2 looks like a PAC, and the rest is all jumbled on top of each other and we can assume that it’s probably a mix of sinus and premature atrial ectopy giving this jumbled stuff (as opposed to atrial fibrillation), and then we see that beat 9 starts a sustained SVT that continues to the end of the strip.
If we look at the moment before each QRS in the new SVT, it looks like there is a P, but with different morphology than the sinus P.
Final Impression?
SVT @ 190 bpm. Likely ectopic atrial tachycardia.
Management implications:
We caught a little bit of atrial ectopy, so with a rate consistent with ectopic atrial tachycardia and what looks like P’ waves before each QRS we can probably call this as an ectopic atrial tachycardia for now. Perhaps one focus that was pumping out PACs just got antsy enough that it is now overdrive-pacing the heart.
Like any SVT if there is critical hemodynamic compromise we will sync shock, or we could try vagals or adenosine or various antiarrhythmics for less urgent situations. Because atrial tachycardias are generally caused by increased automaticity in some atrial focus they often recur after cardioversion or brief interventions like adenosine or vagals, or don’t respond at all.
Get digoxin levels if they take that stuff. Classic AT etiology.
The Take-home Point:
For many tachycardias the heartrate can be a clue as to it’s type. Therefore it’s good to be able to accurately calculate the rate during a burst of tachycardia. The monitor is no good for this if it is brief or paroxysmal because it is always averaging. Therefore, you should be able to make your own calculations.
At high speeds, the difference between one small box extra makes a huge difference in the actual heartrate. For instance, if there are 6 small boxes between QRS complexes the heartrate is 250, and if there are 7 small boxes between complexes the HR is 215. You can’t just eyeball it.
The quick way to get a heartrate at those high speeds is to use the ‘1500’ rule. Count small boxes between complexes. Divide 1500 by that number. In this SVT we see 8 small boxes between complexes so 1500 / 8 = 188bpm.
![]() Two star strip. The meat and potatoes.
Two star strip. The meat and potatoes.