junctional escape rhythm
First Glance:
From across the room it looks like a slow regular narrow-complex rhythm.
Discussion:
First off, it’s regular. Second, it’s narrow. Third, there are no consistent P waves before the QRS’s. So: it’s supraventricular, but is it paced by the atria?
It would be easy to say no because we don’t see convincing P waves, but if I had a dollar for every sinus tracing on the monitor where you couldn’t see the P waves I wouldn’t need to go to med school. We need more info.
If we look closely at the QRS we see little divots just after the S wave, which are most consistent with retrograde P waves, marked with a red triangle below.
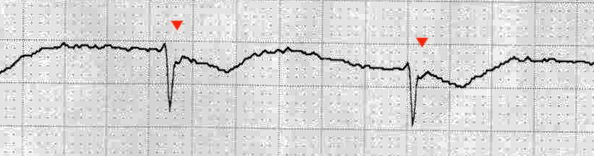
These retrograde P’s are consistent with a junctional rhythm being paced at the AV node. We don’t know what lead this is, but we see the P is negative here, which is consistent with retrograde depolarization of the atria from the AV node going backwards, as would be seen in lead I, II, III, and AVF. The rate is a little over 50 bpm, which is also normal range for a junctional rhythm.
You might be tempted to say this could be sinus with a long first degree block. There are what look like positive P waves before beats 4 and 12, and maybe kinda’ beat 10 and the last beat. But- it doesn’t hold up. At any rate, looking at a little more strip would tell you whether those deflections are random baseline artifact (likely) vs something that really holds up (implying that this is actually sinus rhythm with a poorly visualized P wave).
If you had any doubt about your diagnosis, comparing with a baseline strip would be very helpful. If the sinus QRS complexes look the same as the strip here, but without the negative deflection late in the QRS, you can feel confident these are retrograde P waves.
The T wave is inverted, which might be expected if this was a septal lead, boring as an isolated finding in III, or potentially concerning anywhere else. There might be a little bit of ST depression, but I am reluctant to call it given the superimposed P over the initial ST segment and the poor sensitivity and specificity of tele monitors for ST changes.
Final Impression?
Junctional escape rhythm @ 54 bpm, possibly with T wave inversion.
Management implications:
Generally a perfusing rhythm, but any bradycardia can be symptomatic. This might respond to atropine and sympathomimetics. Causes include diseased hearts and digoxin. If it was dig toxicity, it would be important to reverse the digoxin instead of treating with sympathomimetics to avoid precipitating fibrillatory rhythms, and if the patient was unstable you might preferentially pace them until the digibind was available and working.
If chronic without reversible causes- pacing might be indicated. For now, check lead placement (if this isn’t V1 or V2 then it is more concerning) and evaluate with a 12L. As always, the management implications are extremely dependent on the clinical settings- which isn’t given here.
The Take-home Point:
Don’t limit yourself to looking for P waves solely in front of the QRS.
Retrograde P waves often take a narrow complex and give it some morphologic quirks. An atrial wave superimposed on a QRS can mimic delta waves, bundle branch blocks, and various nonspecific conduction abnormalities.
![]() Two star strip. The meat and potatoes.
Two star strip. The meat and potatoes.