something exciting
First Glance:
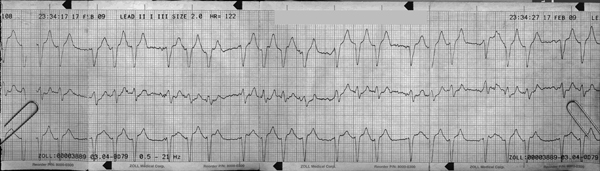
From across the room it looks a wide complex tachycardia with grouped beats.
Discussion:
First off, let’s figure out what we’ve got to work with. This is a Zoll monitor trace of leads II, I, and III reading top to bottom. The printout reads “SIZE 2.0” which means the voltage gain is 200%
There is clear and almost regular grouped beating, generally in groups of three beats with an RR interval that would give you a HR around 150 bpm. There is one group of four beats. The RR distance between each beat within each group is the same, so the third beat is probably not a premature contraction which often gives us grouped beating. That is to say: this is probably not trigeminy.
So either we have some kind of regular atrial rhythm at 150 or 300 bpm that is pacing the ventricles (with a complicated AV block) or perhaps there are bursts of nonsustained VT. The pause between the groups is about 150% of the RR intervals, which made me lean towards a 300 bpm atrial flutter with a variable block. Generally it has a 2:1 block resulting in the 150 bpm rate during the groups, then sometimes it is a 3:1 block resulting in the pauses.
An atrial tachycardia could also do this, but flutter classically runs around this rate, and we can’t see the baseline well enough to make any statements about what the atria are doing.
Unfortunately, to make that tempting diagnosis I’d have to see some atrial activity. Unfortunately, it doesn’t jump out at me here, and even during the pauses I can’t discern anything that really looks like a P or F wave. On a tele box I might be more willing to dismiss this, but this is a defibrillator with excellent quality that can generally produced waveforms on par with a 12L from the floors.
Since we have three leads here we can start to make some decent statements about morphology. We have two inferior leads here (II, III) and both show tiny R waves with deep wide QS waves. This is strongly suggestive of significant axis deviation, consistent with infarction or significant conduction aberrancy.
There is ST elevation in both inferior leads (at a gain of 200%) that is still significant. The ST elevation is more in III.
Final Impression?
Possible SVT (flutter vs AT) with variable block and conduction aberrancy, concerning for active ischemia with infarction, vs persistent nonsustained runs of VT or aberrant SVT, for a ventricular rate of ~115 bpm
Management implications:
Get a 12l rhythm strip (where all leads are printing simultaneously) with the gain cranked up to try to see what is happening during those pauses. If you see P waves, or any regular 300 activity, you can assume this is SVT with an interesting block. Otherwise it’s VT or possibly aberrant SVT. If the 12L does not show a clean atrial rhythm but your suspicion is still high for an atrial paced rhythm, a Lewis lead might show us the light.
That 12L will also evaluate properly for ischemia/infarction. Given the possibility of inferior involvement here, and the increased ST elevation in III with respect to II, this patient should definitely get right sided chest leads to rule out RV infarction. In fact, many would suggest delaying nitroglycerin administration until you have a normal RV4 for fear of bottoming out their preload.
The Take-home Point:
You could argue that you should get right-sided chest leads in any patient with signs of inferior ischemia, but especially so in patients with signs more specific to RV infarction. The ones I am familiar with are:
1) ST elevation III > ST elevation II
2) ST elevation V1 > ST elevation V2
2) ST segment isoelectric in V2 but with ST elevation in V1
![]() Three star strip. Devious stuff.
Three star strip. Devious stuff.