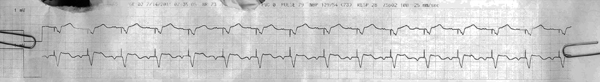
sinus rhythm with ventricular pacing
First Glance:
From across the room it looks like a paced rhythm.
Discussion:
This is a regular rhythm with obvious pacing spikes. Both leads (unlabeled here, but usually II and V on top and bottom, respectively) show P waves, but presumably this patient has significant conduction disease and needs a pacer to keep the ventricles going at a reasonable rate. Based on this strip, the pacer likely senses the atrial depolarization and triggers the ventricle automatically after a set delay (consistent with a DDD pacer with atrial tracking). Every spike is followed immediately by a wide complex QRS, so this is 100% capture.
There is a little ST elevation in both leads. Is this STEMI?
Nope. Moderate amounts of ST elevation in a paced complex is normal, and I refer you to ECGpedia’s review of Sgarbossa’s criteria for the most popular (albeit fairly weak) discussion of EKG signs consistent with ischemia in LBBB and paced rhythms.
Anything else?
Look closely at the P waves in both leads. The upper lead, likely a limb lead, shows bifid P’s with about 40 ms between the peaks. The lower lead, likely a chest lead, shows biphasic positive then negative P waves consistent with a septal lead, with the negative deflection equal to or slightly greater than one small box. However, that is not particularly significant for two reasons. First that the gain is at 160%, and second because the monitor strips may not be calibrated perfectly.
Final Impression?
Atrial-sensed, ventricle-paced rhythm @ ~80 bpm with 100% capture.
Management implications:
If we can assume this is a DDD pacer, it appears that the pacer is working well. To say that a pacer is 100% definitively working correctly would require knowing its pacing mode and settings, however. In this case, it is sufficient to rest assured for now because whether or not the pacer is working exactly as intended, it is probably working well enough. Perhaps tweaking the A->V interval would optimize ventricular filling and subsequent cardiac output, but that is unlikely to be something that would suddenly malfunction, and therefore unlikely something that would be the cause of an acute decompensation.
The Take-home Point:
The paced ventricle morphology changes and it’s interpretation is subsequently difficult to interpret. However, this patient has native P waves here. You should know how to interpret the P wave in V1.
The sinus node is in the right atrium. Therefore the atria depolarize from right to left, generally speaking. Therefore the first half of the P wave is predominantly R atrium, and the second half of the P wave is predominantly L atrium. The normal P wave in V1 is biphasic with an initial positive deflection and then a negative deflection. Therefore, if there is an impressive positive deflection in V1 it is consistent with R atrial enlargement, and if there is an impressive negative deflection in V1 it is consistent with L atrial enlargement.
To call atrial enlargement on a tele strip you will need to have impressive findings. When there is suspicion, don’t over call it. Just get the 12L (or skip it entirely depending on how clinically useful it would be).
![]() One star strip. Students should identify the rhythm correctly.
One star strip. Students should identify the rhythm correctly.