MAT?
First Glance:
From across the room it looks like an irregularly irregular narrow complex tachycardia with some P waves.
Discussion:
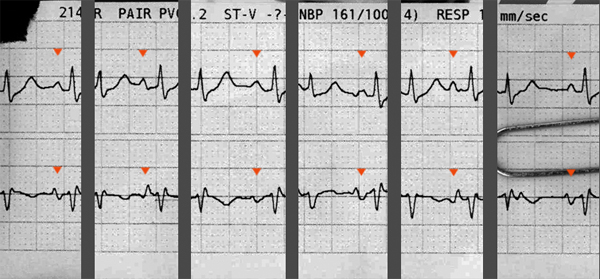
It’s clearly a fast supraventricular tachycardia, but this isn’t afib. If you look carefully, you can clearly pick out P waves before every single QRS. Because they are superimposed over the prior T waves, they are often easier to pick out in the lower lead where the T waves are relatively flat.
The lower lead looks choppy- almost like movement artifact- but it isn’t artifact. The baseline is actually very clean, and I can pick out a few different shapes to the chest lead P waves (mostly sharp biphasic P waves with a positive then negative deflection) which have a normal PR interval. This could be atrial tachycardia. AT usually is regular, but can be irregular (colloquially termed ‘unstable’ AT) even if coming from a single excitable atrial focus.

More commonly in my limited experience an irregular atrial tachycardia is due to competing atrial foci. The trick is to see if the P wave morphology differences are due to truly different foci, or whether it is due to baseline changes or superimposed T waves. If you look in the lower trace, it appears that usually the P wave is positive to negative. Sometimes the P wave is all negative. Sometimes it is all positive. Sometimes it is negative to positive.
The best places to pick out the P morphology is during the longer RR intervals (where the T wave has finished before the P fires in). I copied the longest pauses into this excerpt:
So, we do see various shapes suggesting that various irritable atrial foci are firing. This really could be multifocal atrial tachycardia.
Here is another strip from the same patient, but from a few days before:
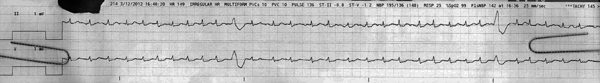
This one is different, and the monitor settings are not as helpful. Here the gain is down in both leads, and we can no longer pick out P waves. The chest lead axis has changed significantly, probably reflecting a more lateral electrode position. There are two similar ventricular beats which come too quickly to be escape beats. This strip is notably less irregular than the first one, so it could be a tachycardic sinus arrhythmia, or PACS, or afib with RVR, or MAT. We can’t tell without a better look at the atrial activity.
Final Impression?
1) Irregular atrial SVT, likely multifocal atrial tachycardia, @ ~170 bpm.
2) SVT @ ~150 bpm with monomorphic PVCs.
Management implications:
This strip is strongly suggestive of MAT, but it’s not 100% definitive. Start with a 12L to confirm the diagnosis.
MAT is associated with right atrial distention and pulmonary disease, and a variety of other clinical disorders. It is less likely to cause hemodynamic compromise than some supraventricular tachycardias because it does have an atrial kick, and the rate does not usually get high enough to cause severe problems.
It is an automaticity arrhythmia, not a reentry arrhythmia, therefore it will not just stop when you break the reentry cycles with a shock. Therefore it is unlikely to respond to cardioversion in the unstable patient. Treat by controlling precipitating factors (R heart strain, electrolytes abnormalities, sympathomimetics, etc) and control rate with beta blockers or calcium channel blockers.
The Take-home Point:
A lead with a clear look at the P waves is the most wonderful thing for deciphering an interesting arrhythmia.
If you have any doubt about this, go back and examine the lower lead very closely. Pick out the native QRS and T wave when it has a little space around it. Then pick out the various P wave morphologies that precede it.
![]() Three star strip. Devious stuff.
Three star strip. Devious stuff.