sinus rhythm
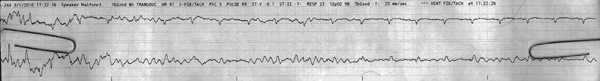
First Glance:
From across the room it looks like movement artifact that resolves in the upper lead to a regular rhythm.
Discussion:
You should be able to spot movement artifact a mile away now. Here we see an incomprehensible choppy trace in both leads, which resolves (especially in the upper lead) to reveal small negative QRS complexes. If you were wondering whether this was VF converting to an organized rhythm- you look at the regular rhythm and trace it backwards. You can see a couple complexes superimposed over the choppy baseline 3 and 4 seconds into the strip.
If you read the top of this strip, the machine says that the “pulse is 89 bpm”. If the choppy artifact was so bad you couldn’t see any QRS complexes, would that “PULSE 89” prove the patient has a pulse?
No. It doesn’t. That is an average of the last however many seconds (depends on the machine). For instance, if the patient had a pulse of 100 bpm and then suddenly went into VF for fifteen seconds- depending on how your machine is calibrated it might print a “pulse rate” of anywhere from 100 to zero bpm. You only know if the patient has a pulse if you 1) feel a pulse, or 2) see a pulse on an arterial catheter waveform or an Sp02 waveform. Those readings are in realtime.
Here is an extension of the same strip:
We can pick out subtle positive P waves before the QRS complexes in many of the later beats in lead II, so this is consistent with a sinus rhythm. Increasing the gain to standard calibration would show these waves better.
Anything else we can get from this? It depends on the lead placement. Here the chest lead was in a septal placement, so the monophasic broad R suggests an incomplete RBBB. We couldn’t call it without more leads, though.
Final Impression?
Sinus rhythm @ ~90 bpm.
Management implications:
Check old QRS morphology. New QRS aberrancy is clinically significant. 12L to evaluate properly.
The Take-home Point:
The monitor calls “VF/VT” for all kinds of choppy artifacts. Sometimes it is bed movement, or loose leads, or chest physical therapy, tremor, seizure, shivering, or agitated/tense patient. Sometimes it is VF/VT. You will become jaded about these alarms (because the monitor “cries wolf” so often), so best get used to looking at the rhythm and rapidly seeing that the alarm is not actually a VF/VT rhythm which would be terminal without rapid intervention.
![]() One star strip. Students should identify the rhythm correctly.
One star strip. Students should identify the rhythm correctly.
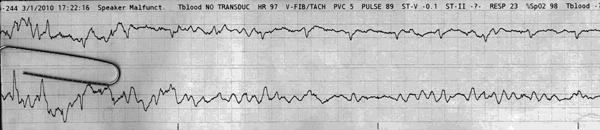
I agree with artifact and clearly not “VFib”. I also agree that there appears to be a seemingly regular narrow-QRS complex at ~85/minute in the upper tracing. However – I would NOT call “P waves” based on anything I see. Statistically – sinus rhythm is by far the most likely diagnosis for a regular supraventricular rhythm at 85/minute – but in my opinion – you can NOT call this based on what I see. I get more of an impression that there ARE sinus P waves on your rhythm extension – but just to realize that what we see is not completely consistent on the extension either – so additional monitoring would be needed (in my opinion) in order to be sure of the rhythm. But – for this strip – I’d say, “LOTS of artifact; fairly regular narrow QRS rhythm at ~85/minute with too much artifact to determine if there is (or is not) atrial activity.