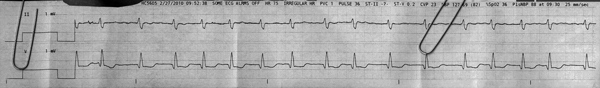
?afib with aberrancy
First Glance:
From across the room it looks irregularly irregular with odd complexes.
Discussion:
Well, it’s irregularly irregular. The gain is down and we don’t see P waves well. If you look closely between beats 3 and 4, and along the baseline of the last 4 beats, you see what could possibly be a flutter baseline at something above 300 bpm. It doesn’t appear to be consistent, nor perfectly regular, so I would lean more towards fib here. It’s less likely to be sinus arrhythmia (with hidden P waves) because the intervals are a little choppy- that is to say there are a series of long RR intervals, then a short one, then a couple long ones, and so on. The best example is the RR interval between beats 9 and 10. That relatively short interval falls smack in the middle of what would have been a slower series in the potential sinus arrhythmia. It just doesn’t fit.
It could always just be sinus with some ectopy if we can’t see the P waves well, and sometimes I can convince myself I might see P waves here. Again, grasping at straws. It’s most likely afib.
Lead II shows a complex that is around 120 ms with a flattened inverted T, and the chest lead shows a significant Q wave (>40ms and 2mm tall at 50% gain) with a wide R, some ST depression, and either a biphasic T or an inverted T with a U wave. If the chest lead is a septal lead this is consistent with RBBB, or without RBBB it is concerning for RVH or right heart strain with ischemia. If this is a lateral lead this is concerning for infarction and ischemia. If this was somewhere in the middle it might just be nonspecific IVCD, but we still would wonder about anterior ischemia.
Did you notice the Sp02 reading that printed out? 36%? What does that mean?
It depends. It the pulse ox sensor is on a finger, it could be reading artificially low. Check the waveform- if it doesn’t look pulsatile and lovely the number the monitor spits out is worthless. And even if the waveform looks good, numbers below around 70% are not reliable. All you know is that the saturation on that finger is low. How low is anybody’s guess.
Final Impression?
Wide complex afib @ ~75 bpm, likely RBBB.
Management implications:
Gain the monitor up a lot to try to see what the atria are doing. There is a world of difference between afib and sinus arrhythmia, and you want to be sure you’re getting it right.
Check Sp02 waveform and reposition sensor if necessary. Check old strips/12Ls to see if the wide complex is new. 12L to assess for ischemia and infarction, and to evaluate atrial activity if you didn’t pick it up on the monitor.
The Take-home Point:
A low Sp02 can have many causes. First, it could be a low saturation. But it could also be a low-flow state with peripheral blood that has deoxygenated far below the central saturation, or a loose sensor that is reading artifact, or it could be caused by one of the various confounders of pulse oximetry (although these are generally unlikely to change the reading significantly downwards).
Sp02 sensors that aren’t getting good readings in the hypotensive or cold patient are a constant battle for me. Here are some neat tricks.
![]() One star strip. Students should identify the rhythm correctly.
One star strip. Students should identify the rhythm correctly.