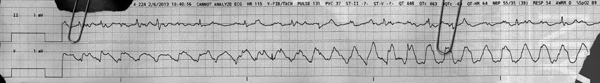
regular narrow-complex rhythm with PVCs
First Glance:
From across the room it looks like VT vs artifact.
Discussion:
Fine. You got me. This is another artifact strip, where something is giving the marked artifact in the lower lead. The frequency of this artifact is around 2 Hz- lower than respiratory PT vibration, so I’m not actually sure what is generating this. It’s regularity suggests a mechanical or electrical device. Invasive equipment like IABPs and CVVH equipment can sometimes cause interesting artifacts like this, but I don’t have the answer in this case. The point here is to practice differentiating artifact from rhythm, and reading through the artifact.
In the lower lead we see apparent wide regular complexes. The rate on those complexes is about 140. You could get this strip from VT or some SVT with aberrancy. The upper lead doesn’t have the tall wide complexes (with only small bifid positive deflections associated with each big complex), and it also has irregularly irregular positive deflections that look like they could be QRS complexes. Sometimes the artifact looks like them- we don’t know clearly which ones are real and which ones might be artifact by morphology. How about if you see if they could be regular with some dropped beats?
See here:

This excerpt above starts about 3 seconds into the upper lead. We can clearly march out similar-looking QRS’s (magenta), but with two apparent dropped beats (blue). The next magenta beat is right on time, and we can see that before each dropped beat (blue) there is a similar-looking negative deflection followed by a wide positive deflection. These are probably PVCs with a compensatory pause.
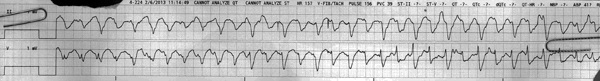
Let’s look at a strip from the same patient when the artifact is not there.
Now we can see that those positive spikes in the upper lead (II) are definitely native, although we can’t tell from this strip whether there are associated P waves. We do see that they are narrow with a regular rate under 40 bpm. This sounds like a junctional rhythm, but we can’t be sure here. Gaining the lead up would help.
Now the artifact is back. What do you see?
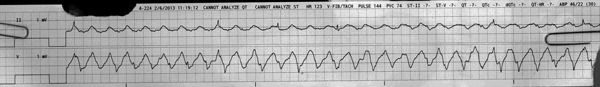
The artifact is back. We can see the native QRS’s in the upper lead, but at what rate? This looks irregularly irregular and slow. I only count six beats in about 12 seconds, which is a rate of 30 beats per minute. The upper trace looks clean enough that I would expect to see the QRS’s (or other ectopy), so I believe this pt is actually going that slow.
Look at their ABP. MAP of 30.
The monitor printed this strip because it thought the pt was in VT/VF. we know better than that. The monitor said the pulse was 144. We know better than that (the Sp02 or ABP is probably picking up the same artifact as the EKG). We might be tempted to look at the monitor, see that it thinks this is VT, and dismiss the alarm because we know that is wrong. But a second looks shows that they are severely bradycardic with a low BP. Pay attention!
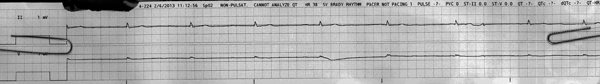
Here we see so much artifact in both leads that I no longer feel confident picking out QRS’s. I have no idea how this person is doing. The monitor is unsure about their invasive BP and is giving ridiculous numbers for their HR and pulse. This is effectively an unmonitored patient.
What I do see is two sharply negative spikes midway through the upper lead. These look like a bit like pacer spikes. I can’t tell whether there is capture, nor can I guess why a pacer might be firing now. It may also be artifact. Time to get to the bedside and investigate.
Final Impression?
1) Regular narrow-complex rhythm @ ~60 bpm with monomorphic PVCs with compensatory pauses
2) Regular narrow complex bradycardia @ 38 bpm
3) Markedly bradycardic irregular supraventricular rhythm @ ~30 bpm
4) Uninterpretable rhythm.
Management implications:
You don’t really know what you’re dealing with here. Do what you need to do to figure it out.
The Take-home Point:
Sometimes you need to read EKGs over artifact. While trying to decipher a whole minute of rhythms on top of artifact is a stretch (you would try to find what is causing it, and turn if off, right?) it’s not an unseen situation. What if telemetry recorded a possible concerning EKG event while the chest PT was running? You might still want to figure out what it was.
What is it was something that you couldn’t turn off? An oscillator vent? A balloon pump? Electric interference from a bedside device that isn’t functioning properly? What if the patient is shivering or seizing or agitated? You’d just have to read through the artifact.
While we will always try to get pristine strips, sometimes it’s worth practicing with the funky stuff so we have some facility when the shit hits the fan.
![]() Three star strip. Devious stuff.
Three star strip. Devious stuff.